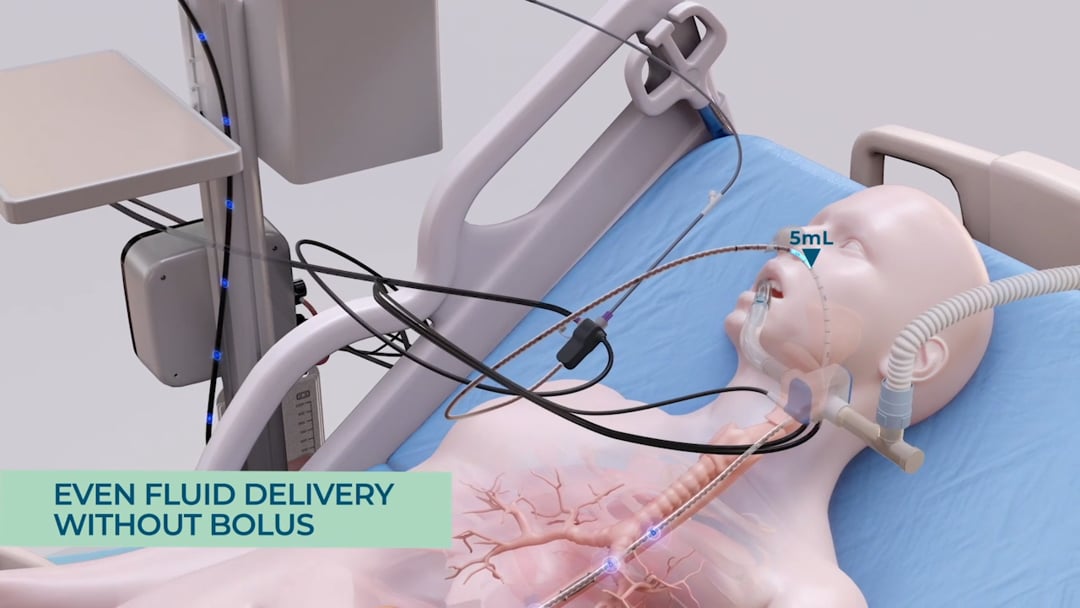
Reflux and Aspiration Prevention
In the United States alone, an estimated one million patients are affected by ventilator-associated events annually. Pneumonia is the most common infection in Intensive Care. A study of 329 ventilated and tube fed patients from 2010 showed that 88% had at least one event of gastric content aspiration during the three days monitored [1].
In cases of feeding intolerance, stomach content builds up and gastric pressure rises, causing the patients to experience a series of reflux events, often unbeknownst to the clinical staff. If gastric matter travels past the lower esophageal sphincter up the esophagus and the patients continue to be ventilated, the gastric content may be aspirated into the lungs. This puts the patients at a very high risk for ventilator-associated-pneumonia.
With the smART+ platform, reflux events are automatically detected and prevented in real-time using a sensor-based feeding tube. The sensors on the feeding tube detect and log the natural history of the patients’ reflux events. The algorithm processes the data collected by the sensors and enables the system to take immediate and automatic actions to prevent aspiration from occurring. A thin, lightweight balloon located on the feeding tube inflates automatically and thus stops any gastric content from moving up the esophagus. At the same time, the GRV pressure release mechanism is activated: the system automatically pauses feeding, so as to not increase the pressure by adding more feeding material to the stomach. This is followed by the opening of a port which enables any excess gastric content to be released into a GRV bag. This is done using only the natural gastric pressure inside the stomach – no suction is employed. This way the system ensures that only excessive gastric content is evacuated. As a result, the pressure inside the stomach is reduced and the reflux can subside.
[1] Metheny, N., Davis-Jackson, J., & Stewart, B. (2010). Effectiveness of an Aspiration Risk-Reduction Protocol. Nursing Research, 59(1), 18-25. doi: 10.1097/nnr.0b013e3181c3ba05.


 Global Site
Global Site