Calculating Patient Energy Needs
Mechanically ventilated patients are unable to take food orally and therefore are dependent on enteral nutrition for provision of both energy and protein requirements. Many critically ill patients often have pre-existing conditions, including malnutrition. All of this predisposes patients to nutrition deficits, muscle wasting, delayed wound healing, slower recovery, and increased risk of morbidity and mortality.
Providing adequate energy via nutrition support to the mechanically ventilated patient is critical. In the mechanically ventilated patient, overfeeding, even for short periods of time, can lead to hyperglycemia and increases time on the ventilator. On the other hand, an increasing caloric deficit (persistent underfeeding) may also increase time on the ventilator.
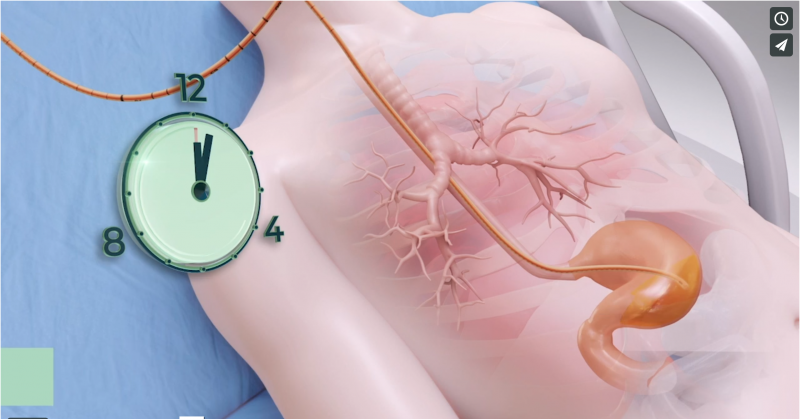
Indirect calorimetry is the recommended method of determining patients’ resting energy expenditure (REE). However, a 2015 estimate showed that only 2% of ICUs in the United States regularly employed indirect calorimetry. Predictive equations have therefore been the most commonly practiced method of determining energy needs. The literature, however, clearly indicates that each equation has a large potential for error. This makes it difficult to accurately predict an individual patient’s energy requirements during critical illness. In general, predictive equations estimate accurately only 50% of the time in ICU patients.
The ASPEN/ESPEN guidelines demonstrate that such inaccuracies affect short term mortality and infection complications.
54% of ICU patients are malnourished. Current methods are unable to deliver the required amount of nutrients to the patient, causing on average six additional days of hospitalization and 50% more likelihood to return to the hospital within 30 days of discharge.[1]
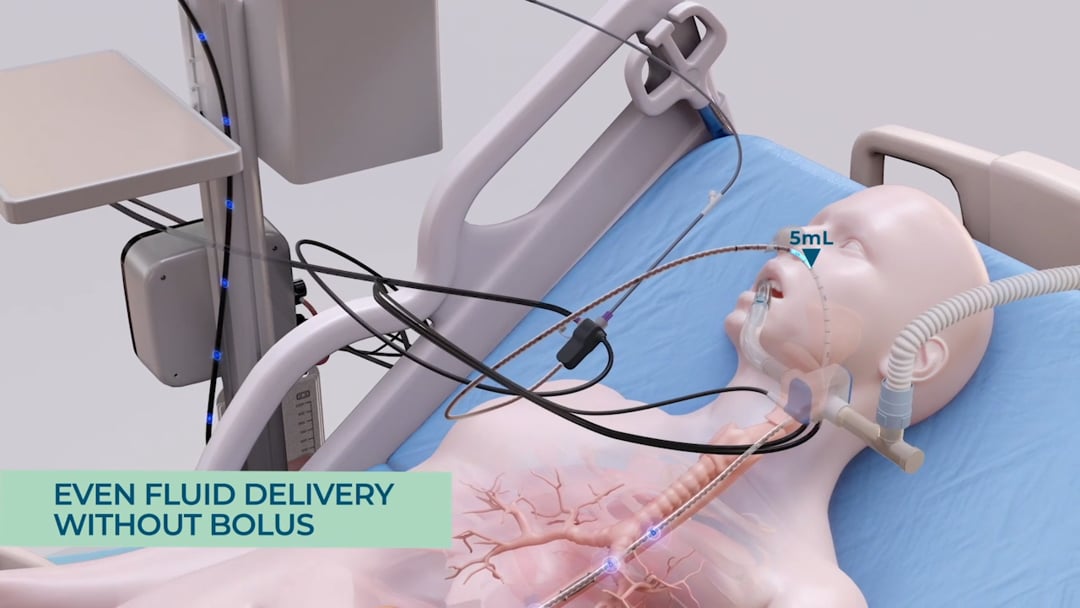
The smART+ platform automatically calculates the patient’s REE (resting energy expenditure) while providing continuous, cost-effective, per-patient monitoring. The system tracks any metabolic fluctuations in real-time, and changes in the patient’s energy expenditure are recorded automatically. If the resting energy expenditure changes, the system recalculates the patient’s feeding needs, automatically updating the volume of nutrition to be delivered.
The smART+ Platform automates and continuously calculates patients’ energy requirements, reducing the risk of errors from manual calculations. This provides a reliable foundation for an optimal and personalized nutrition plan, which the platform calculates and administers automatically.
[1] Allen, K., & Hoffman, L. (2019). Enteral Nutrition in the Mechanically Ventilated Patient. Nutrition In Clinical Practice, 34(4), 540-557. doi: 10.1002/ncp.10242.


 USA Site
USA Site